| Prompt | Response | Req | Len |
|---|---|---|---|
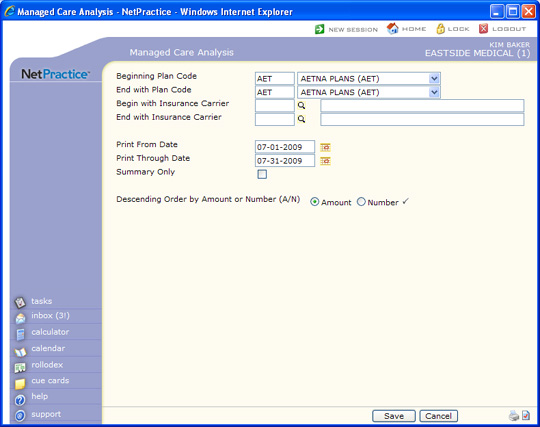
| Beginning Plan Code | Type the code you want to begin with, select from the list, or leave the field blank to start with the first plan code in the table. | 5 | |
| End with Plan Code | Type the code you want to end with, select from the list, or leave the field blank to end with the last code in the table. | 5 | |
| Begin with Insurance Carrier | Type the code you want to begin with, click the magnifying glass to search the table, or leave the field blank to start with the first code in the table. | 5 | |
| End with Insurance Carrier | Type the code you want to end with, click the magnifying glass to search the table, or leave the field blank to end with the last code in the table. | 5 | |
| Print From Date | Type the Accounting Date you want to start with or click the calendar icon to select a date. | 10 | |
| Print Through Date | Type the Accounting Date you want to end with or click the calendar icon to select a date. | 10 | |
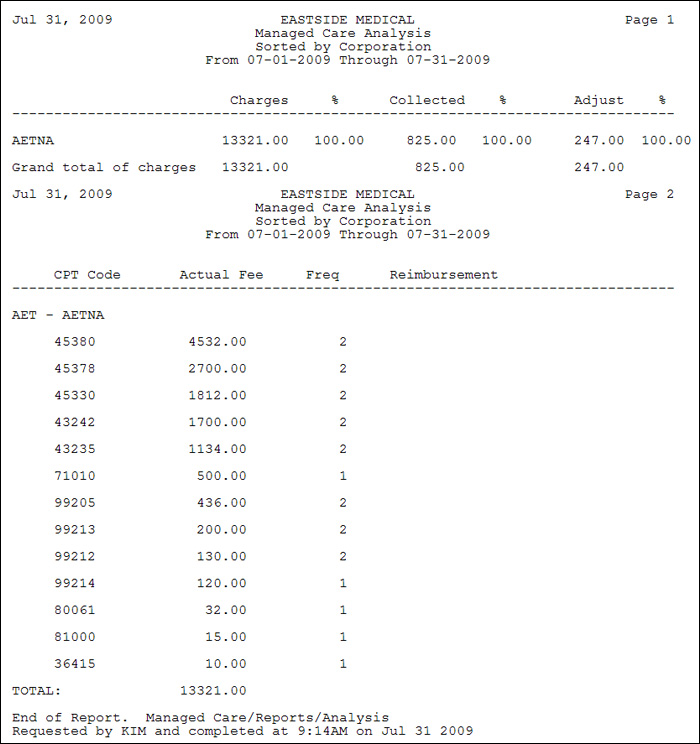
| Summary Only | If you only want to print a summary for each carrier without the individual CPT code detail, select this check box. |  |
1 |
| Descending Order by Amount or Number (A/N) | Select the option to indicate the order you want to use to print the report. The Amount option represents the total charges billed, and if you select this option, the insurance carriers are listed in order starting with the highest billed amounts. The Number option represents the total number of charges billed (Frequency), and if you select this option, the insurance carriers are listed in order starting with the highest number of charges. NOTE: The CPT detail section of the report is optional and can be very lengthy depending on the number of carriers included in the report. |
 |
1 |