| Prompt | Response | Req | Len |
|---|---|---|---|
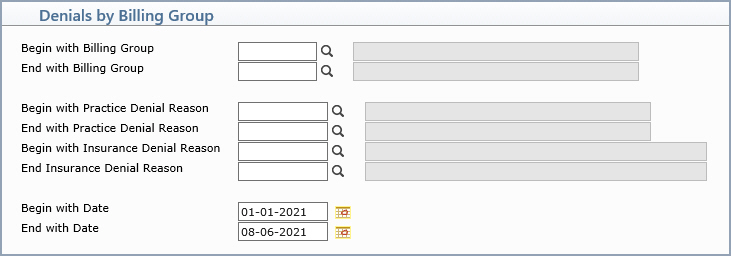
| Begin with Billing Group | Type the code you want to begin with, click the magnifying glass to search the table or leave the field blank to start with the first code in the table. | 8 | |
| End with Billing Group | Type the code you want to end with, click the magnifying glass to search the table or leave the field blank to end with the last code in the table. | 8 | |
| Begin with Practice Denial Reason | Type the code you want to begin with, click the magnifying glass to search the table or leave the field blank to start with the first code in the table. | 10 | |
| End with Practice Denial Reason | Type the code you want to end with, click the magnifying glass to search the table or leave the field blank to end with the last code in the table. | 10 | |
| Begin with Insurance Denial Reason | Type the code you want to begin with, click the magnifying glass to search the table or leave the field blank to start with the first code in the table. | 10 | |
| End with Insurance Denial Reason | Type the code you want to end with, click the magnifying glass to search the table or leave the field blank to end with the last code in the table. | 10 | |
| Begin with Date | Type the date you want the report to start with or click the calendar icon to select a date. This date is referring to the date the procedures were denied, not the actual date of service. | 10 | |
| End with Date | Type the date you want the report to end with or click the calendar icon to select a date. This date is referring to the date the procedures were denied, not the actual date of service. | 10 |