| Prompt | Response | Req | Len |
|---|---|---|---|
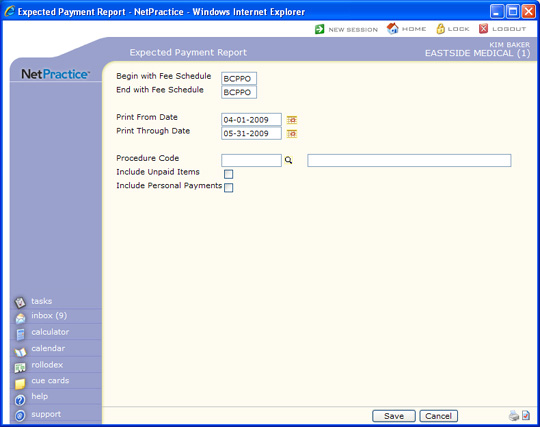
| Begin with Fee Schedule | Type the code you want to begin with or leave the field blank to start with the first code in the table. | 5 | |
| End with Fee Schedule | Type the code you want to end with or leave the field blank to end with the last code in the table. | 5 | |
| Print From Date | Type the Accounting Date you want the report to begin with or click the calendar icon to select a date. | 10 | |
| Print Through Date | Type the Accounting Date you want the report to end with or click the calendar icon to select a date. | 10 | |
| Procedure Code | Type the code you want, click the magnifying glass to select a code, or leave the field blank to include all codes. | 10 | |
| Include Unpaid Items | If you want to include unpaid charges, select this check box. If you select this check box, the report includes charges posted with an Accounting Date within the selected date range that have no payments posted to them. It will include any adjustments posted to those charges. | 1 | |
| Include Personal Payments | If you want to include personal payments, select this check box. The personal payments print under the PERS fee schedule. Co-payments are included as personal payments on this report. | 1 |