| Prompt |
Response |
Req |
Len |
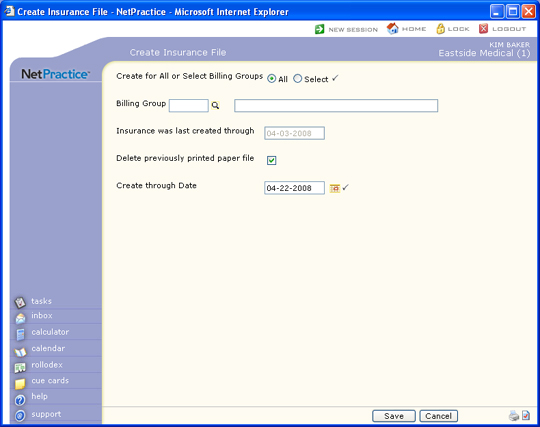
| Create for All or Select Billing Groups |
Select the Billing Group option you
want to create the insurance file. |
 |
1 |
| Billing Group |
If you chose to create the insurance
file for a Select Billing Group only, type the code you want or
click the magnifying glass to search the table. |
|
5 |
| Insurance was last created through |
This field is informational only and
reflects the date that the insurance file was last created. |
|
10 |
| Delete previously printed paper file |
If you want to delete the previously
printed paper file, select this check box. If you select this
check box, all claims that are in the paper claim file that have
already been printed, will be deleted. If there are claims in
the print file that have not been printed, they will not be deleted.
This will not affect the electronic claims submission file. |
 |
1 |
| Create through Date |
Type the date you want or click the
calendar icon to select a date. This date refers to the accounting
date that the charges were posted with. Any charge with an accounting
date after this date, will remain in patient responsibility and
will not have a claim generated. |
 |
10 |