| Prompt | Response | Req | Len |
|---|---|---|---|
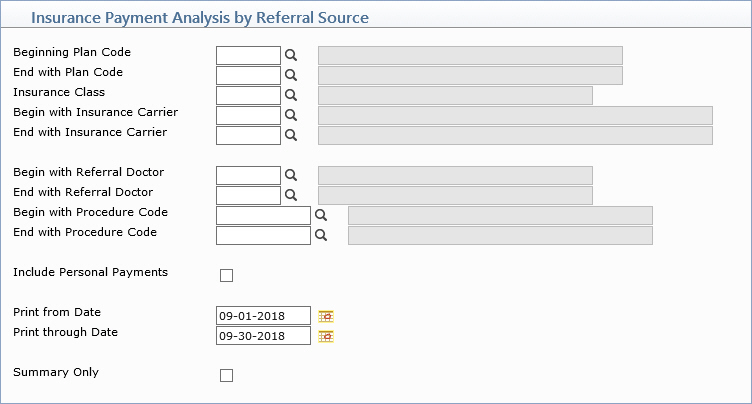
| Beginning Plan Code | Type the code you want to begin with, select from the Plan Code list, or leave the field blank to start with the first code in the table. | 5 | |
| End with Plan Code | Type the code you want to end with, select from the Plan Code list, or leave the field blank to end with the last code in the table. | 5 | |
| Insurance Class | Type the code you want, select from the Insurance Class list, or leave the field blank to include all codes in the table. | 5 | |
| Begin with Insurance Carrier | Type the code you want to begin with, click the magnifying glass to search the table, or leave the field blank to start with the first code in the table. | 5 | |
| End with Insurance Carrier | Type the code you want to end with, click the magnifying glass to search the table, or leave the field blank to end with the last code in the table. | 5 | |
| Begin with Referral Source Code | Type the code you want to begin with, select from the Referral Source list, or leave the field blank to start with the first code in the table. | 5 | |
| End with Referral Source Code | Type the code you want to end with, select from the Referral Source list, or leave the field blank to end with the last code in the table. | 5 | |
| Begin with Procedure Code | Type the code you want to begin with, click the magnifying glass to search the table, or leave the field blank to start with the first code in the table. | 10 | |
| End with Procedure Code | Type the code you want to end with, click the magnifying glass to search the table, or leave the field blank to end with the last code in the table. | 10 | |
| Include Patient Pmts/Adj | If you want to include patient payments and adjustments applied to charges on this report, select this check box. | 1 | |
| Print from Date | Type the Accounting Date you want the report to begin with or click the calendar icon to select a date. | 10 | |
| Print through Date | Type the Accounting Date you want the report to end with or click the calendar icon to select a date. | 10 | |
| Summary Only | If you want to print a summary only, select this check box. | 1 |