Populate Collection Roster
The Insurance Collections Module revolves around status codes. The
status codes are static and cannot be changed.
- Insurance Denial
- Timely Filing
- Expected Payment Days
- Pending
- Timely Filing and Expected Payment Days
The Populate Collection Roster function is the key function for Insurance
Collections. It determines which claims enter the collection process,
the migration path for claims already in the collection process, and it
removes claims from the collection process that are no longer delinquent.
This function can be performed manually or you can have it automatically
performed on a nightly basis by CGM webPRACTICE. The automatic roster
population option is set in the Insurance
Collections Integration located on the System, Database Maintenance
Menu.
The Populate Collection Roster function:
- Evaluates each open (unpaid) item in the insurance balance on the
patient accounts, not already in the collection process, to see if
they meet the criteria to enter the collection process and at which
status. This is done based on the criteria set in the Insurance
Carrier Table for that carrier. If nothing is entered there, it
will look at what was entered in the Insurance Collections Integration.
It also evaluates accounts already in the collection process to see
if they need to be transferred to another status.
- Insurance Denial Status: If a claim has been denied
it moves into the Denial status. If that denied claim is
subsequently refiled, it is not moved into the collections module.
If there is a denial that is marked as a Patient denial, it is
ignored.
- Timely Filing Status: This will compare the date the
claim was originally filed to the date of service. If the difference
is greater than what the Timely Filing is set to for that
carrier, it will move into the Timely Filing status.
- Expected Payment Days Status: If a claim has not been
paid within the Expected Payment Days set for that carrier,
it will populate into the Expected Payment Days status.
- Pending Status: You can pend claims automatically when
you work the collection accounts, or if an Insurance Collection
letter has been printed, the populate will move the claim into
the Pending status and attach a follow-up date as specified
in the Insurance Carrier Table or the Insurance Collections Integration.
- Timely Filing and Expected Payment Days Status: Some
claims, depending on the timeframe of the criteria that you set,
may fall into both the Timely Filing and Expected Payment
Days status.
- Removes accounts that no longer meet these criteria from the collection
process.
- Evaluates which insurance carrier owes the balance on each item.
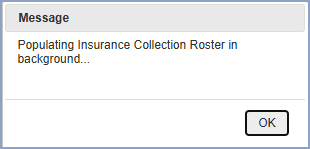
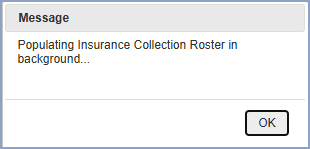
Upon accessing this function, the populate process will start immediately.
Click OK when the message appears informing you the population
will be performed in the background. This means the job will perform independently
and you do not have to stay in this function until it is complete.
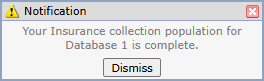
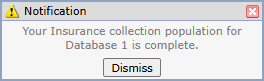
You can continue with other tasks and CGM webPRACTICE displays a message
in the upper-left corner of the screen when the population of the collection
roster is complete. NOTE: The message will not display until the
screen is 'refreshed' by you clicking on another function or menu.
If you choose to manually populate the collection roster:
- You MUST take care to ensure the populate function is run at the
appropriate intervals so that claims move into the correct statuses
at the right time depending on the time lines you've set.
- You should ALWAYS print your letters the same day your perform
the populate.
If you choose the automatic roster population every night, you should work
your accounts daily using the Work Accounts function, and you should print
your letters daily. This will ensure the appropriate letters are generated
for each claim and that each claim receives the proper attention while
migrating through the collection process.
After you populate the collection roster you can then Print
Collection Roster.