DMERC Setup Process
If your office sells take-home supplies, you need to perform the following steps to conform to Medicare's requirements to send Durable Medical Equipment Regional Carrier (DMERC) claims from CGM webPRACTICE.
Step 1 - Contact EMEDIX
EMEDIX will instruct whether or not you need to contact the DMERC for your region and will perform any set up steps that need to be completed for your practice to begin sending DMERC claims electronically.
NOTE: If you need to send DMERC paper claims instead of DMERC electronic claims, contact the DMERC for your region to see if it is necessary to register to send claims to them and then complete Steps 2-5.
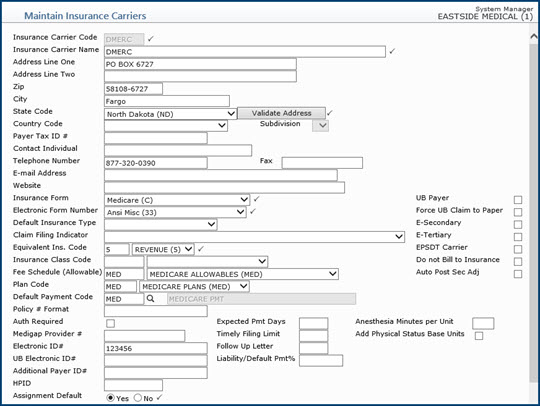
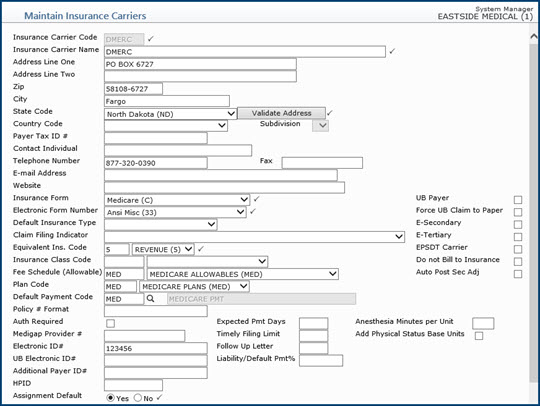
Step 2 - Create a DMERC Insurance Carrier
Using the Maintain Insurance Carriers function located on the Tables, Insurance Carrier Table menu, create a DMERC Insurance Carrier. To find the correct carrier for your region, refer to the DMERC Contact Information section.
NOTE: Do not add the DMERC carrier as an insurance carrier on the patient's account.
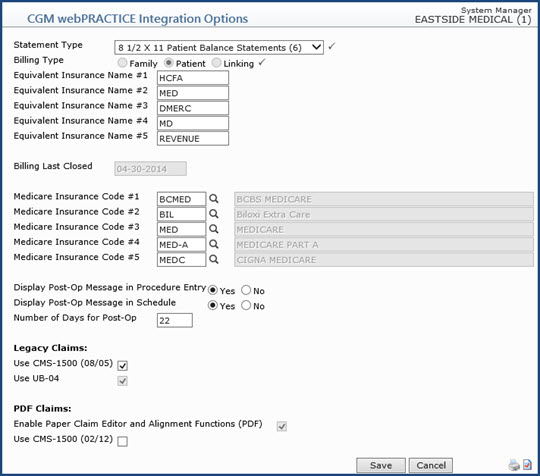
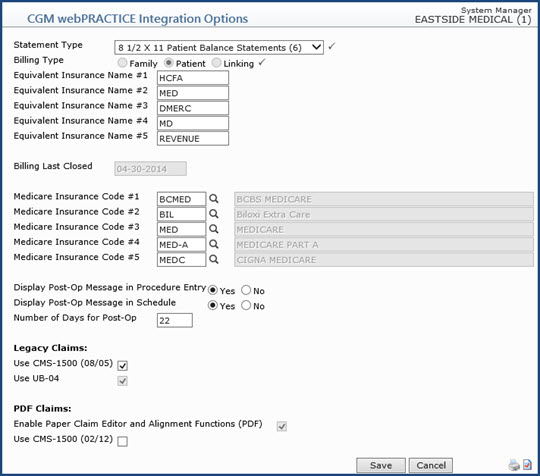
Step 3 - Update CGM webPRACTICE Integration Options
Set up a DMERC equivalent insurance and all of your Medicare insurance codes in CGM webPRACTICE Integration Options located on the System, Database Maintenance Menu. In one of the Equivalent Insurance Name # fields, type DMERC or the exact DMERC insurance carrier code that you set up in Step 2.
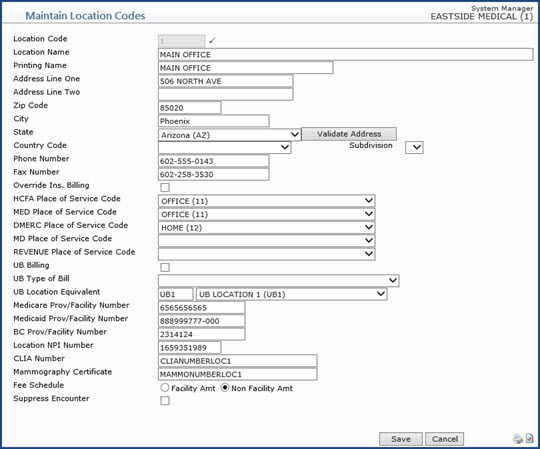
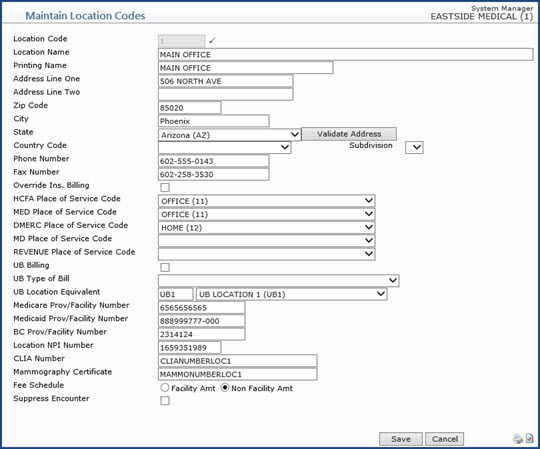
Step 4 - Update the Location Code Table
Set up a DMERC-equivalent Place of Service code for all locations from which you sell take-home supplies, in Maintain Location Codes on the Tables, Location Code Table menu. In the DMERC Location Code field, type 12, which is the Place of Service code for the Patient's Home.
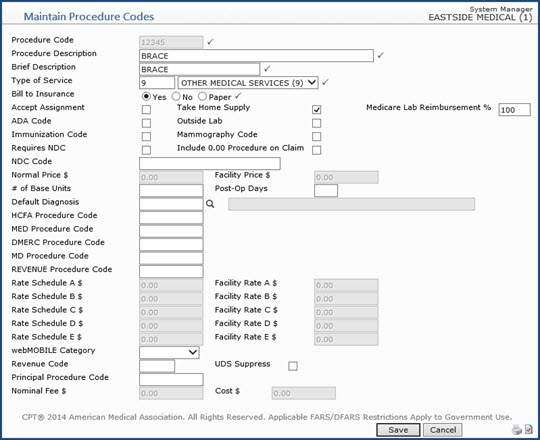
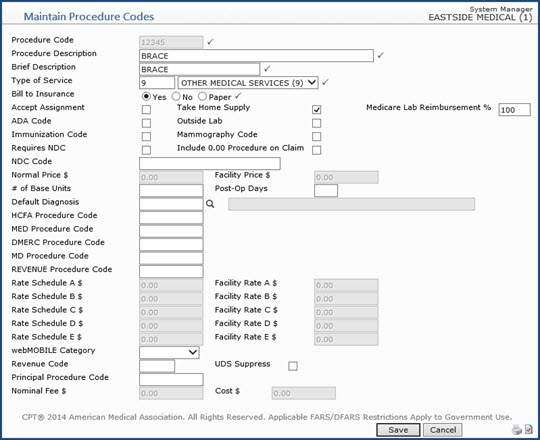
Step 5 - Update the DMERC Procedure Codes
Using the Maintain Procedure Codes function located on the Tables, Procedure Code Table menu, edit every procedure code that is considered to be a 'Take Home Supply'. For each procedure code, select the Take Home Supply check box. CGM webPRACTICE will then be able to separate out the DMERC claims and file them to DMERC.
DMERC Contact Information
- Region A
NHIC, Corp.
Claims Addresses: Contact carrier - addresses vary based on claim type for paper claims.
NHIC's Contact Information
Customer Service: 866-590-6731
Interactive Voice Response (IVR) Phone: 866-419-9458
website: http://www.medicarenhic.com/dme/
Serving: Connecticut, Delaware, District of Columbia, Maine, Maryland, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island and Vermont
- Region B
National Government Services
Claims Addresses: Contact carrier - addresses vary based on claim type for paper claims.
National Government Services Contact Information
Customer Service: 866-590-6727
Interactive Voice Response (IVR) Phone: 877-299-7900
website: http://www.ngsmedicare.com
Serving: Illinois, Indiana, Kentucky, Michigan, Minnesota, Ohio, and Wisconsin
- Region C
CGS Administrators, LLC (CGS)
CGS's Contact Information
Claims Address: CGS Administrators, LLC (CGS) PO Box 20010 Nashville, TN 37202
Customer Service: 866-270-4909
Interactive Voice Response (IVR) Phone: 866-238-9650
website: http://www.cgsmedicare.com/jc/index.html
Serving: Alabama, Arkansas, Colorado, Florida, Georgia, Louisiana, Mississippi, New Mexico, North Carolina, Oklahoma, Puerto Rico, South Carolina, Tennessee, Texas, Virginia, West Virginia and the US Virgin Islands
- Region D
Noridian Healthcare Solutions
Noridian Healthcare Solutions' Contact Information
Customer Service: 877-320-0390
Interactive Voice Response (IVR) Phone: 877-320-0390
website: https://www.noridianmedicare.com/web/jddme/
Serving: Alaska, American Samoa, Arizona, California, Guam, Hawaii, Idaho, Iowa, Kansas, Missouri, Montana, Nebraska, Nevada, North Dakota, Northern Mariana Islands, Oregon, South Dakota, Utah, Washington and Wyoming