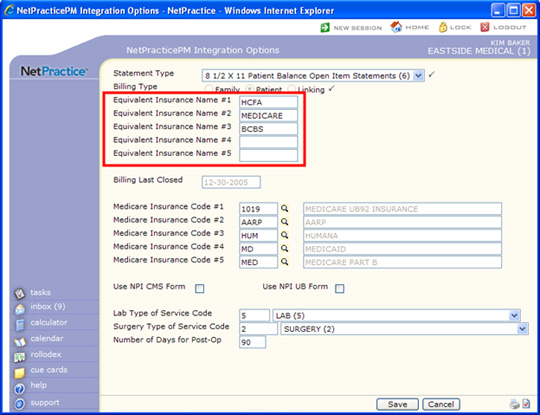
Equivalent Codes
CGM webPRACTICE enters the Equivalent Code field names when your database
is set up. The field names entered are the ones most commonly used, but
you can change them in CGM
webPRACTICE Integration Options.
- Equivalent Insurance Name #1 = HCFA: This is a generic code
to be used for all insurance carriers or situations that do not require
a specific equivalent code. You can change the name of this
field, but this field has specific programming tied to it and cannot
represent a specific insurance company. The name should always represent
the broadest, most general category encompassing all claims.
- Equivalent Insurance Name #2 = MEDICARE: You can change
this field name, if necessary, to represent another insurance
carrier that you may have equivalent codes for.
- Equivalent Insurance Name #3 = BCBS: You can change this
field name, if necessary, to represent another insurance carrier
that you may have equivalent codes for.
- Equivalent Insurance Name #4 and #5 = Unassigned: These
fields are left unassigned and you can add insurance carrier names
if necessary.
You can use Equivalent Codes for a variety of reasons. For example,
you would use the HCFA (general) equivalent code fields for Practice-Specific
Codes if your practice uses particular codes for ease of posting,
tracking, or reporting but still needs the correct billing code to go
on the insurance claims. In this case you would enter the correct billing
code in the HCFA Equivalent Code field in the appropriate table.
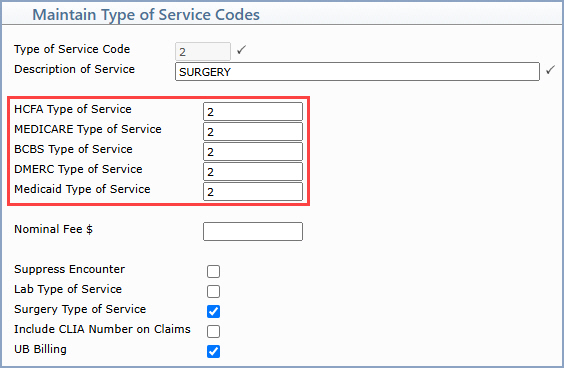
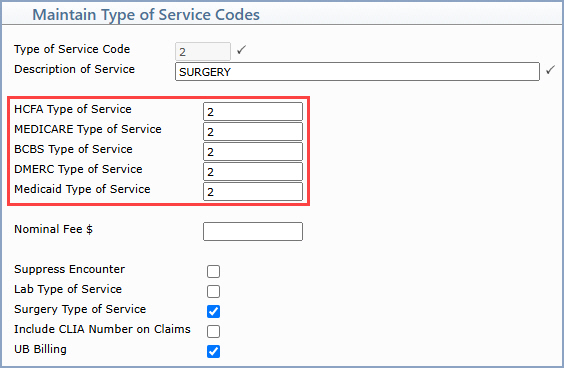
For example, you could have a separate practice-specific Type of Service
code for each radiology service (X-Ray, MRI, Ultrasound). All of these
should normally be billed with the standard Radiology Type of Service
code of 4. So, in the Type of Service Table you would create
an MRI Type of Service Code and type 4 in the HCFA Type
of Service field, so on all of the procedure codes that have that
MRI Type of Service attached CGM webPRACTICE places that correct
Type of Service code of 4 on all of your electronic and paper claims.
But, when you run your reports by Type of Service, you can see the detail
under each of your radiology categories rather than them just being condensed
together under the Radiology (4) Type of Service.
You would use the four remaining carrier-specific equivalent fields for
Insurance-Required Equivalent Codes where a particular insurance
company requires codes that are different from the standard billing codes
dictated by the Centers for Medicare and Medicaid Services (CMS). For
example, CMS's CPT code for Venipuncture is 36415, but you may have an
insurance carrier that uses their own internal list of codes and they
may define 'Venipuncture' as 'G0001'. So in the Procedure Code Table
for 36415, you would type G0001 in the MEDICARE Procedure Code
field.
Complete the following steps to set up equivalent codes in your system
where needed:
- Verify the Equivalent Codes in CGM
webPRACTICE Integration Options.
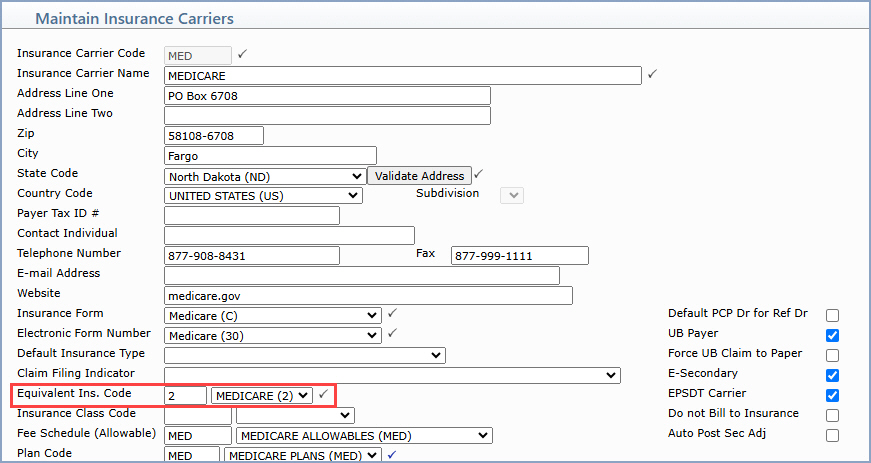
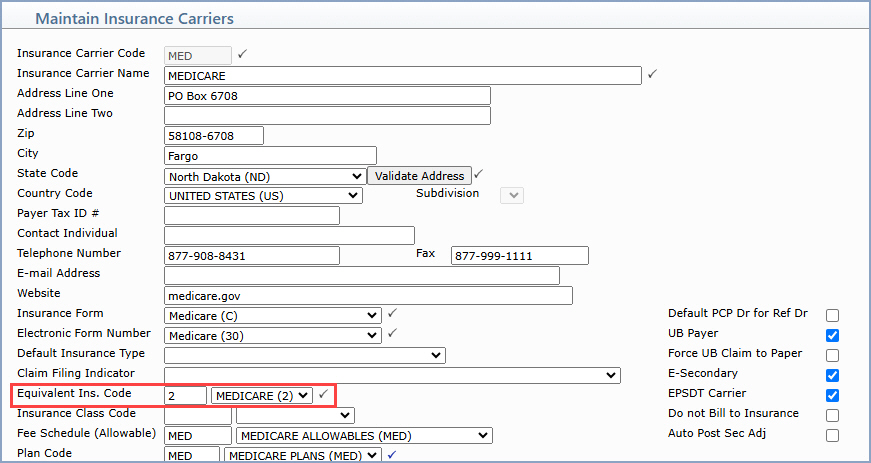
- Attach the Equivalent Insurance Names to the Carriers
in Maintain
Insurance Carriers.
- The Equivalent Ins. Code field is a CGM webPRACTICE
required field. If you use equivalent codes for this carrier,
select the corresponding Equivalent Code category from the list.
For example, if you have a Medicare equivalent insurance
carrier name because all of the Medicare programs require a specific
equivalent type of service code, you need to link the Medicare
equivalent name to all of your Medicare carriers by selecting
Medicare in the Equivalent Ins. Code field. If you
do not use equivalent codes for this carrier, select the HCFA
(or the generic) category from the list. What you select here
controls which equivalent codes, if any, are submitted on your
claims.
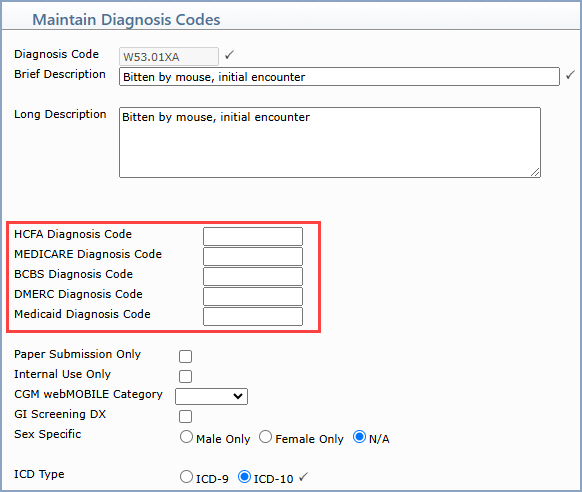
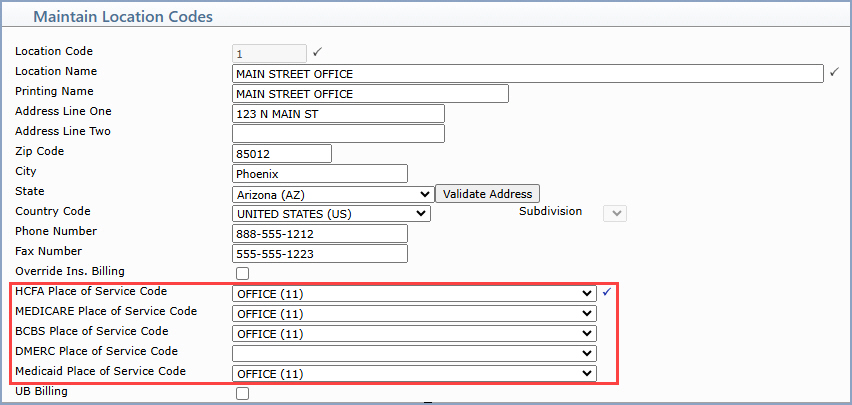
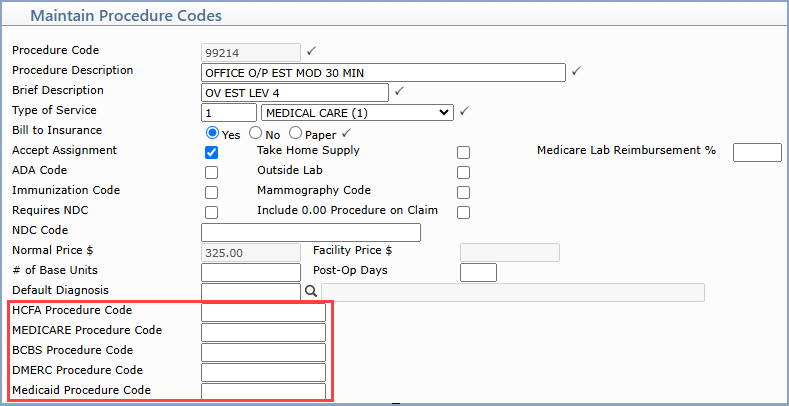
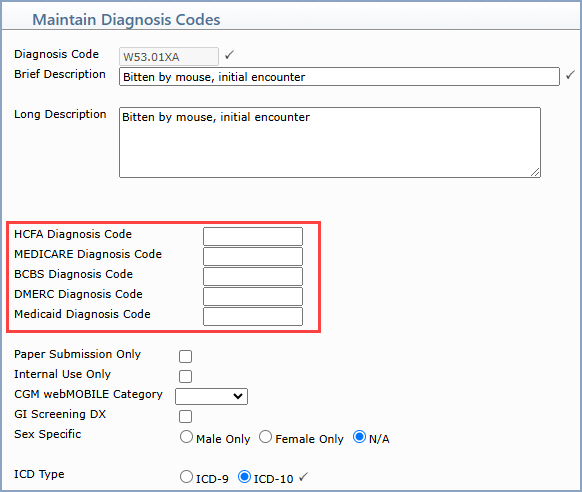
- Enter the Equivalent Codes in the Tables
- The equivalent code field names that you defined in CGM webPRACTICE
Integration Options reflect as the equivalent code field titles.
- Type the equivalent code in the appropriate field(s) for each code
and carrier that requires an equivalent code.
- NOTE: If you enter any equivalent codes in any of
the tables, CGM webPRACTICE pulls the codes onto the claims in a specific
way: If you enter a carrier-specific equivalent code, that code is
pulled onto the claim. But, if the carrier-specific equivalent field
is blank, then whatever is in the HCFA equivalent field pulls onto
the claim. If both the carrier-specific and the HCFA equivalent
fields are blank, the standard code pulls onto the claim.
- Diagnosis Code Table
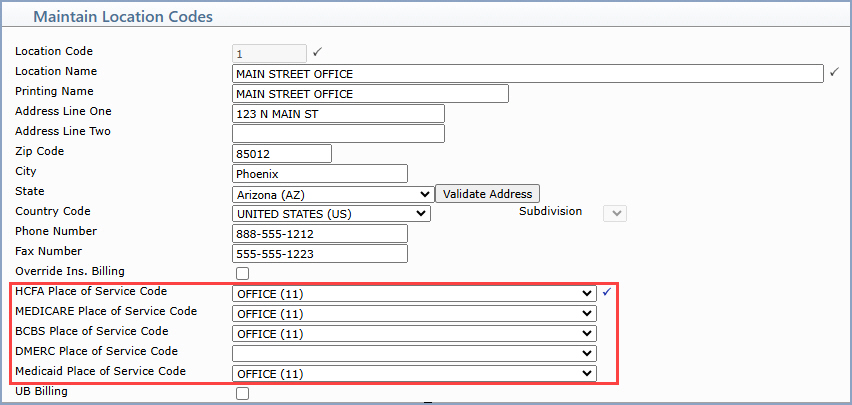
- Location Code Table
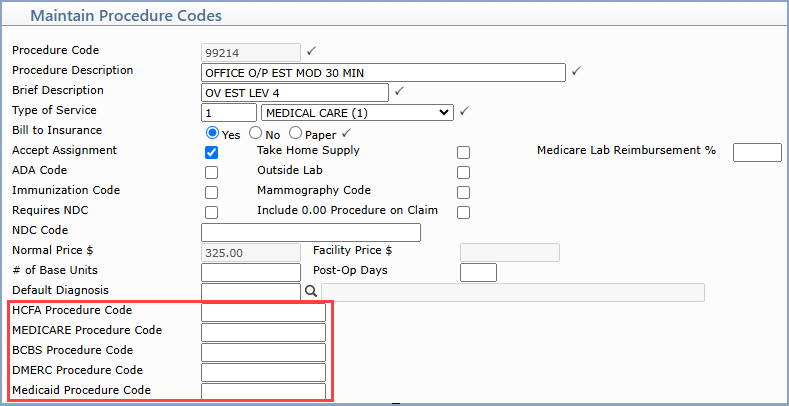
- Procedure Code Table
- Type of Service Table
Procedure Entry
When you enter charges in the Procedure
Entry Function, enter the standard codes. If the tables and codes
are set up properly, when the claim is printed or sent electronically,
CGM webPRACTICE pulls the correct equivalent codes onto the claim. Only
the standard codes reflect in the patient's transaction history; the equivalent
codes do not display anywhere except for on the claim.